Your Trusted Source for All Things Related to Wet Age-Related Macular Degeneration (Wet AMD)
Learn all about this eye condition, including its symptoms, risk profiles, when to see a doctor, how it’s diagnosed, as well as treatment options.
It is normal that we experience changes in our vision as we age. One progressive eye condition that affects people over 50 is Age-related Macular Degeneration (AMD).
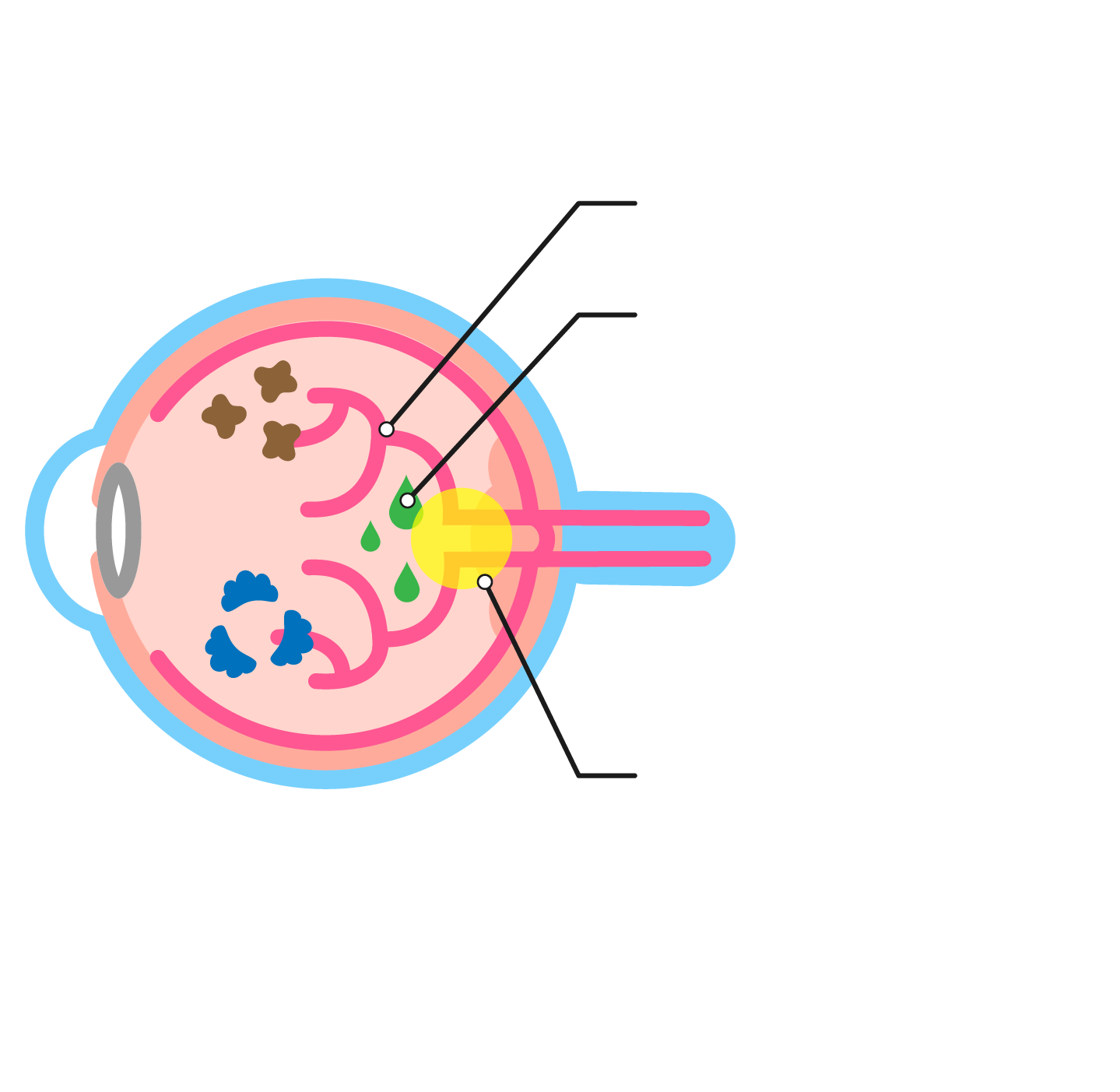
AMD targets the macula (the central part of the retina responsible for sharp, clear vision).
This can result in blurry or distorted vision, and central vision loss in more severe cases.⁽ ¹ ⁾ ⁽ ² ⁾
What is Wet AMD?
Wet AMD is a more advanced form of AMD occurs when abnormal blood vessels grow under the macula.
This growth of abnormal blood vessels is a key feature of wet AMD, ⁽ ¹ ⁾ and is caused by a protein called vascular endothelial growth factor (VEGF), a signal protein produced by many cells that is responsible for the formation of blood vessels.
These abnormal blood vessels may leak blood and other fluids into the back of your eye, including the macula, the area responsible for clear central vision.⁽ ² ⁾
NOTE: Wet AMD does not mean your eye is more teary! The word “wet” is a scientific term used to describe the abnormal blood vessels leaking fluid into the retina.
What are the Symptoms of Wet AMD?
How do you know if you or your loved one has wet AMD? Unlike dry AMD, symptoms of wet AMD can develop suddenly (as quick as a day) or progress over time. ⁽ ³ ⁾ They usually affect one eye first before possibly involving the other eye. ⁽ ⁴ ⁾
Here are the most common symptoms of wet AMD to look out for: ⁽ ² ⁾
Central vision loss (dark spots)
Wet AMD affects the central part of the retina responsible for sharp, detailed vision. Hence, people with wet AMD may notice a dark or empty area (scotoma) in the centre of their vision, while their side or peripheral vision (vision at the outer field) remains intact.


Reduced colour perception / Decreased contrast sensitivity
In some cases, when the cones (light receptor cells responsible for colour vision) are affected, you may perceive colours to be less vibrant or more washed out. ⁽ ⁵ ⁾
You may find it tough to see objects against their background or tell between different levels of brightness. ⁽ ⁶ ⁾


Blurred or distorted vision
You may notice that your vision starts to get blurred or distorted and unclear.


Straight lines appearing wavy
Do you see straight lines appearing wavy or curved? This happens because the macula — the central part of the retina responsible for detailed central vision — is affected by the growth of abnormal blood vessels in wet AMD.


Rapid worsening of symptoms
Unlike dry AMD, which usually progresses slowly, wet AMD can cause rapid vision loss within days or weeks. ⁽ ⁷ ⁾
Normal Vision
Vision Distortion is an early symptom of wet AMD
Wet AMD decreases sensitivity to contrast
Advanced wet AMD will create a permanent blind spot in your central vision
Who should I contact if I notice my vision is getting worse?
If you or your family members experience any of these symptoms or sudden changes in vision, do promptly consult an eye care professional. Early diagnosis and treatment can help slow the progression of wet AMD and potentially preserve your vision.
Who is at Risk of
Wet AMD?
Your risk of developing wet AMD may be higher if you:
- have a family history of AMD
- are aged 50 or older
- smoke. Smokers are four times more likely to develop AMD than non-smokers ⁽ ⁸ ⁾
- have heart disease ⁽ ⁹ ⁾ or high blood pressure ⁽ ¹⁰ ⁾
- are female ⁽ ¹¹ ⁾
- are obese ⁽ ¹² ⁾
In Asia, roughly 0.56% of people between the ages of 40 to 79 have or are at risk of developing wet AMD. ⁽ ¹³ ⁾ There are several subtypes of wet AMD worldwide, but in Asia, polypoidal choroidal vasculopathy (PCV) is the predominant subtype. ⁽ ¹⁴ ⁾
Your doctor will take the necessary steps to ensure you are accurately diagnosed, to ensure you get the right treatment you need. ⁽ ¹⁴ ⁾ ⁽ ¹⁵ ⁾ ⁽ ¹⁶ ⁾

When to See an Eye Doctor for Wet AMD
You should have an eye examination as part of your regular health check-up. If you have AMD, it’s important to get your eye checked often. This is because: ⁽ ⁴ ⁾
- AMD can worsen over time
- Early treatment may help to slow down progression of AMD
- If you have AMD in one eye, you might develop it in the other eye too.
Do consult an eye specialist immediately if you experience any of these symptoms: ⁽ ¹⁷ ⁾
- Any change in vision or sudden blurriness
- New floaters or flashes in your vision
- Double vision
- Sudden loss of vision
Do speak with your doctor about how often you should get your eyes checked.
How is Wet AMD Diagnosed?
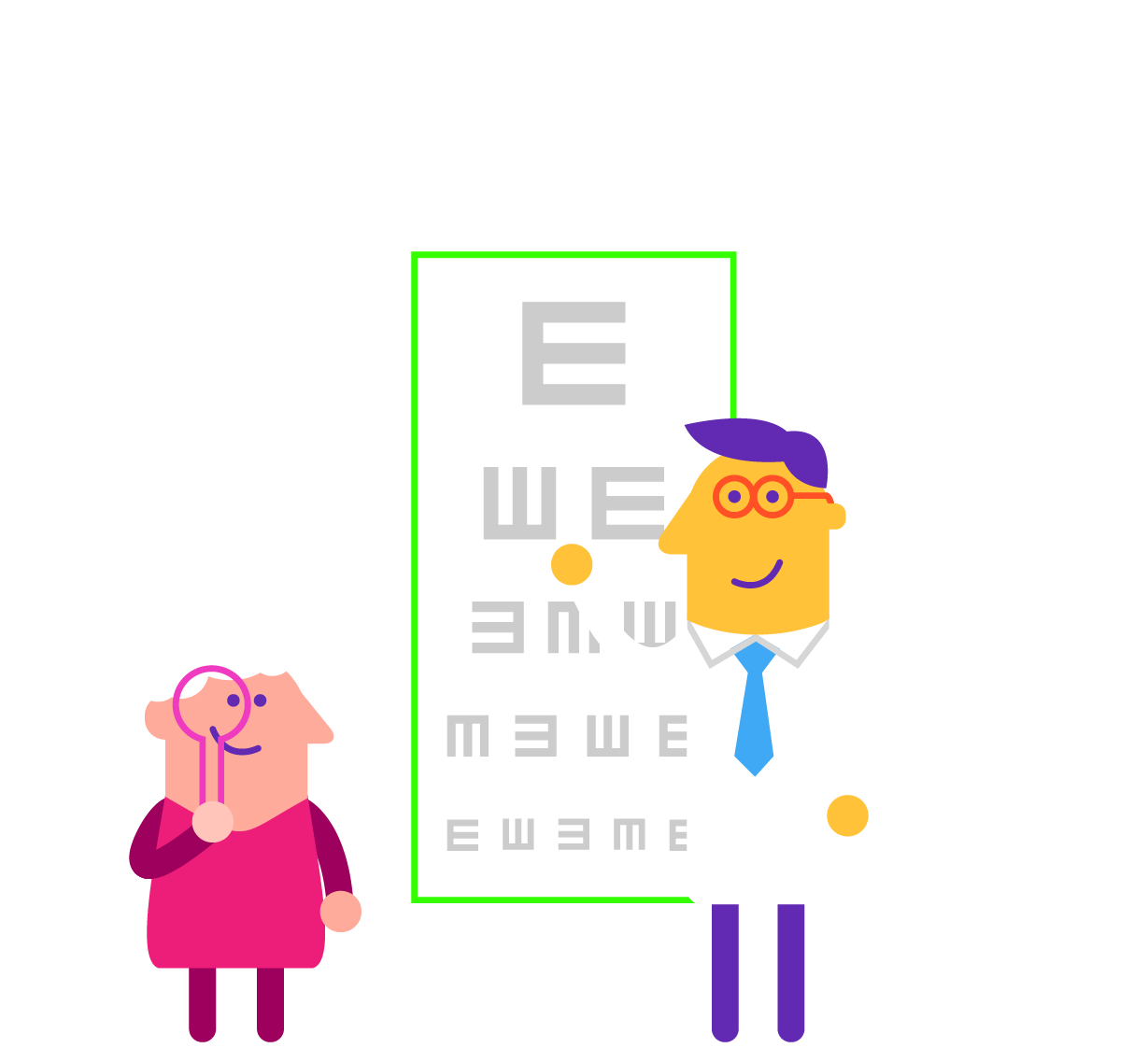
To diagnose wet AMD, your eye doctor will first have a chat with you about your health history, including your eye health and family history.
They will then perform an eye examination, which may include the following tests: ⁽ ² ⁾
- Visual acuity test: An eye chart is used to measure how clearly you can see at different distances.
- Retina examination: A test to check the back of your eye to see if there’s any blood, fluid or drusen (tiny yellowish deposits).
- Central grid (Amsler grid) test: A test to check for any issues with central vision.
- Optical Coherence Tomography (OCT): An imaging test that provides detailed images of your retina.
- Indocyanine green angiography (ICGA): This test is used to further differentiate between the types of wet AMD.
Not all patients will undergo the same tests, your doctor will decide which tests to include as part of your eye examination.
Wet AMD
Treatment Options
The good news is there are treatment options available for wet AMD than can slow down the disease and stop your vision from getting worse. It’s important to speak to your doctor about which treatment options might work best for you. ⁽ ² ⁾
The main treatment option for wet AMD is
Intravitreal Anti-VEGF Therapy
- Anti-VEGF therapy is the gold standard in the treatment of wet AMD, and has been shown to slow down disease progression, and potentially save your vision. ⁽ ¹⁸ ⁾
- The treatment typically involves injecting the anti-VEGF medication directly into the affected eye or eyes. ⁽ ¹⁸ ⁾
- Commonly used anti-VEGF drugs approved by HSA Singapore include aflibercept, ranibizumab and faricimab. Faricimab is a new drug that works by blocking both VEGF and Angiopoietin-2 (Ang-2) to prevent leakage and swelling in the eye. ⁽ ¹⁹⁾ (Ang-2 is another protein involved in blood vessel formation).
- It is important to note that anti-VEGF therapy does not cure wet AMD, it slows progression of the disease.
Your doctor may or may not recommend these secondary treatment options,
depending on your condition:
Nutritional supplements
to reduce
Wet AMD progression
The AREDS2 formula is a specific combination of vitamins and minerals that may help slow the progression of AMD. The AREDS2 formula contains the following: ⁽ ²⁰ ⁾
- Copper
- Lutein
- Vitamin C
- Vitamin E
- Zeaxanthin
- Zinc oxide
Photodynamic Therapy for Wet AMD
A treatment option that combines the use of a laser and light-sensitive medication. This treatment is only recommended for very specific patients depending on their condition. ⁽ ²¹ ⁾ ⁽ ²² ⁾
Laser Surgery for Wet AMD
A treatment option that aims to seal off the leaking blood vessels that cause vision problems in wet AMD. This treatment is only recommended for very specific patients depending on their condition. ⁽ ²³ ⁾
References:
- [1] Wet Age-related Macular Degeneration (Wet AMD). NIH. National Library of Medicine. StatPearls Publishing. Available at www.ncbi.nlm.nih.gov/books/NBK572147/. Accessed on 5 April 2023.
- [2] WebMD – What is wet age-related macular degeneration? Available at www.webmd.com/eye-health/macular-degeneration/wet-amd-what-is. Accessed on 5 April 2023.
- [3] BrightFocus Foundation. Symptoms of Wet Age-Related Macular Degeneration (AMD). Available at https://www.brightfocus.org/macular/article/symptoms-wet-age-related-macular-amd#:~:text=The%20symptoms%20of%20the%20vision,gray%2C%20red%2C%20or%20black. Accessed on 29 May 2023.
- [4] SightMatters. Working with your doctors. Available at www.sightmatters.com/article-detail-topics/work-with-your-doctors/. Accessed on 10 April 2023.
- [5] Vemala, R, et al. Detection of early loss of color vision in age-related macular degeneration – With emphasis on drusen and reticular pseudodrusen. Invest Ophthalmol Vis Sci 2017;58(6):BIO247-BIO25.
- [6] Wai KM, et al. Contrast sensitivity function in patientswith macular disease and good visual acquity. Br J Ophthalmol 2022;106:839-844.
- [7] Ask the Expert: Can You Slow or Reverse Wet AMD Progression? Available at https://www.healthline.com/health/slow-or-reverse-wet-amd-progression. Accessed on 27 April 2023.
- [8] FDA.gov. Health Effects of Tobacco Use. How Smoking Can Contribute to Vision Loss and Blindness. Available at www.fda.gov/tobacco-products/health-effects-tobacco-use/how-smoking-can-contribute-vision-loss-and-blindness. Accessed on 10 April 2023.
- [9] Moutsinai.org. Press Release: Blinding eye disease strongly associated with serious forms of cardiovascular disease. Available at https://www.mountsinai.org/about/newsroom/2022/blinding-eye-disease-strongly-associated-with-serious-forms-of-cardiovascular.
- [10] Xu X, et al. Hypertension, antihypertensive medications use and risk of age-related macular degeneration in California Teachers Cohort. J Hum Hypertens 2020;34(8):568-576.
- [11] Ross C, et al. Conversion rates from non-exudative to exudative age-related macular degeneration: An AAO IRIS Registry Analysis. Invest Ophthalmol Vis Sci 2022;63:3118.doi.
- [12] Zhang QY, et al. Overweight, obesity and risk of age-related macular degeneration. Invest Ophthalmol Vis Sci 2016;57:1276-1283.
- [13] Kawasaki R, et al. The prevalence of age-related macular degeneration in Asians: a systematic review and meta-analysis. Ophthalmology 2010;117(5):921-927.
- [14] Retinatoday.com. March 2022 Global Perspectives. Differentiating PCV from wet AMD. Available at https://retinatoday.com/articles/2022-mar/differentiating-pcv-from-wet-amd. Accessed on 10 April 2023.
- [15] Yuzawa M, et al. The origins of polypoidal choroidal vasculopathy. Br J Ophthalmol 2005;89(5);602-607. Accessed on 28 April 2023.
- [16] Yanagi Y, et al. Asian age-related macular degeneration: from basic science research perspective. Eye (Lond) 2019;33(1):34-49.
- [17] American Academy of Ophthalmology – 20 reasons to see an ophthalmologist. Available at https://www.aao.org/eye-health/tips-prevention/why-ophthalmologist-eye-exam-2020-vision. Accessed on 10 April 2023.
- [18] Lanzetta P, et al. Fundamental principles of an anti-VEGF treatment regimen: optimal application of intravitreal anti–vascular endothelial growth factor therapy of macular diseases. Graefes Arch Clin Exp Ophthalmol 2017; 255(7): 1259–1273.
- [19] Vabysmo.com. How Vabysmo works. Available at: https://www.vabysmo.com/wamd/how-vabysmo-works.html. Accessed on 10 April 2023.
- [20] AREDS 2 Supplements for Age-Related Macular Degeneration (AMD). Available at https://www.nei.nih.gov/learn-about-eye-health/eye-conditions-and-diseases/age-related-macular-degeneration/nutritional-supplements-age-related-macular-degeneration. Accessed on 23 May 2023.
- [21] Clinical effectiveness and cost-utility of photodynamic therapy for wet age-related macular degeneration: a systematic review and economic evaluation. Available at https://www.ncbi.nlm.nih.gov/books/NBK62326/. Accessed on 23 May 2023.
- [22] Photodynamic Therapy for Age-Related Macular Degeneration. Available at https://www.hopkinsmedicine.org/health/treatment-tests-and-therapies/photodynamic-therapy-for-agerelated-macular-degeneration. Accessed on 27 April 2023.
- [23] Laser Photocoagulation for Age-Related Macular Degeneration. Available at https://www.hopkinsmedicine.org/health/treatment-tests-and-therapies/laser-photocoagulation-for-agerelated-macular-degeneration. Accessed on 27 April 2023.